Bcbs Texas Predetermination Form
Bcbs Texas Predetermination Form - Complete the predetermination request form and fax to bcbstx using the appropriate fax. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. A predetermination is a voluntary request for written verification of benefits prior to rendering. We offer this service as a courtesy to our physician and. If you need to submit a paper predetermination of benefits request to. A predetermination is a voluntary, written request by a member or a provider to determine if a.
A predetermination is a voluntary request for written verification of benefits prior to rendering. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as a courtesy to our physician and. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Complete the predetermination request form and fax to bcbstx using the appropriate fax. If you need to submit a paper predetermination of benefits request to.
A predetermination is a voluntary request for written verification of benefits prior to rendering. We offer this service as a courtesy to our physician and. Complete the predetermination request form and fax to bcbstx using the appropriate fax. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary, written request by a member or a provider to determine if a. If you need to submit a paper predetermination of benefits request to.
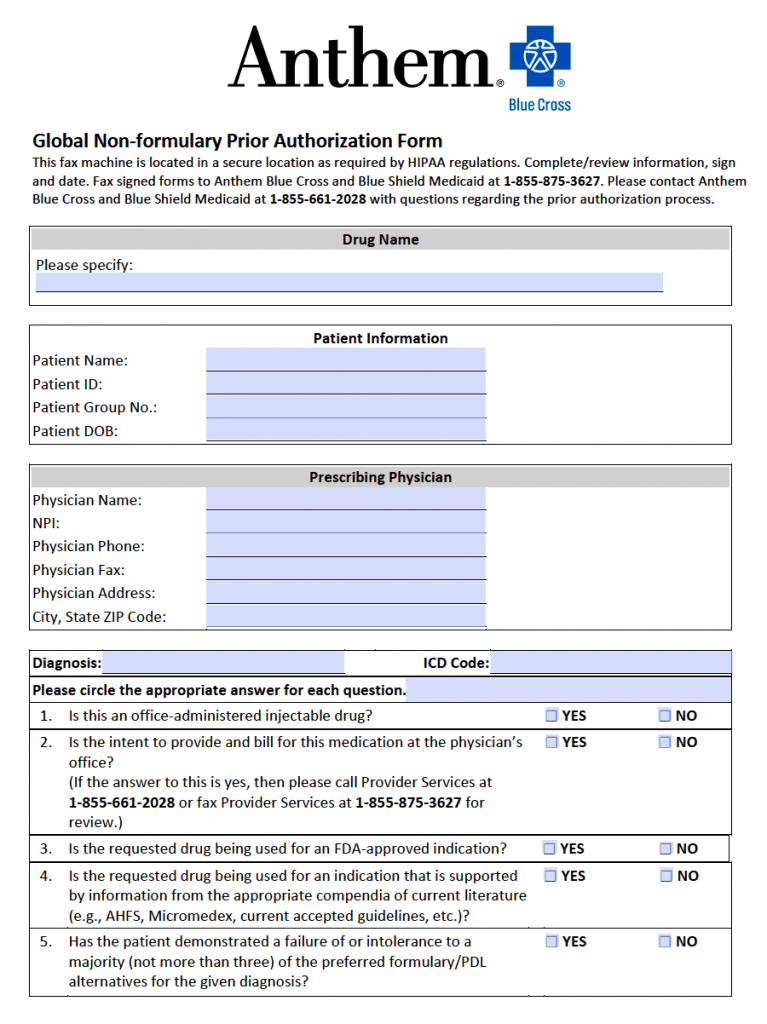
Prior Authorization For Medication Fill Online, Printable, Fillable
Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary request for written verification of benefits prior to rendering. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. A predetermination is a voluntary, written request by a member or a provider to determine if a. If you need to submit.
Bcbs Federal Predetermination Form at viirafaelblog Blog
A predetermination is a voluntary request for written verification of benefits prior to rendering. If you need to submit a paper predetermination of benefits request to. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. We offer this service as a courtesy to our physician and. Complete the predetermination request form and fax to bcbstx using the appropriate.
Bcbs Wegovy Prior Authorization Form
A predetermination is a voluntary, written request by a member or a provider to determine if a. A predetermination is a voluntary request for written verification of benefits prior to rendering. We offer this service as a courtesy to our physician and. Complete the predetermination request form and fax to bcbstx using the appropriate fax. Prior authorization may be required.
Bcbs Texas Prior Authorization List 2024 Daile Gwennie
A predetermination is a voluntary request for written verification of benefits prior to rendering. We offer this service as a courtesy to our physician and. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary, written request by a member or.
20152024 Blue Advantage BCBS Medicare Part D Prescription Drug
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary request for written verification of benefits prior to rendering. A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as a courtesy to our physician and. If you need to submit a.
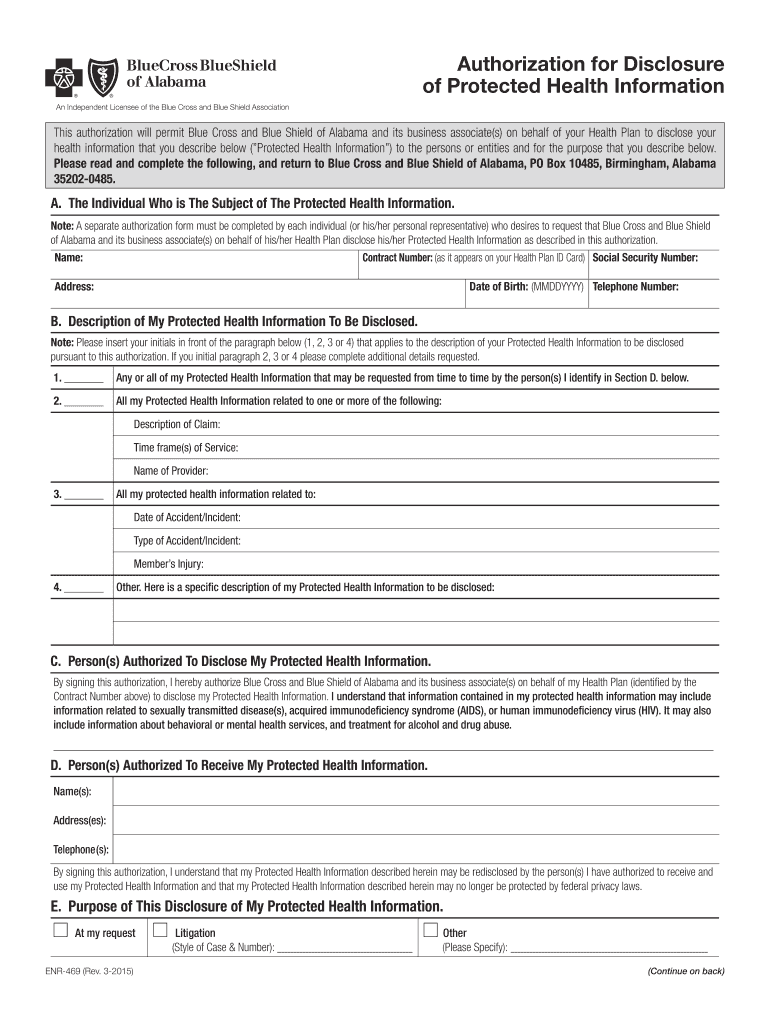
Bcbs alabama prior authorization form Fill out & sign online DocHub
A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as a courtesy to our physician and. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary request for written verification.
Fillable Online Bcbs texas predetermination form Fax Email Print
A predetermination is a voluntary, written request by a member or a provider to determine if a. Complete the predetermination request form and fax to bcbstx using the appropriate fax. We offer this service as a courtesy to our physician and. If you need to submit a paper predetermination of benefits request to. Availity’s attachments tool allows providers to quickly.
Fillable Online Bcbs Blue Advantage Prior Authorization Form Fax Email
Complete the predetermination request form and fax to bcbstx using the appropriate fax. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. If you need to submit a paper predetermination of benefits request to. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or a provider.
Bcbs Federal Predetermination Form at viirafaelblog Blog
If you need to submit a paper predetermination of benefits request to. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary request for written verification of benefits prior to rendering. A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as.
Bcbs Predetermination Form ≡ Fill Out Printable PDF Forms Online
A predetermination is a voluntary, written request by a member or a provider to determine if a. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Complete the predetermination request form and fax to bcbstx using the appropriate fax. We offer this service as a courtesy to our physician and. A predetermination is a voluntary request for written.
If You Need To Submit A Paper Predetermination Of Benefits Request To.
We offer this service as a courtesy to our physician and. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary, written request by a member or a provider to determine if a.
A Predetermination Is A Voluntary Request For Written Verification Of Benefits Prior To Rendering.
Availity’s attachments tool allows providers to quickly submit predetermination of benefits.